INTRAHEPATIC CHOLANGIOCARCINOMA (BILE DUCT CANCER)
Dr. Nikhil Agrawal
Intrahepatic bile duct
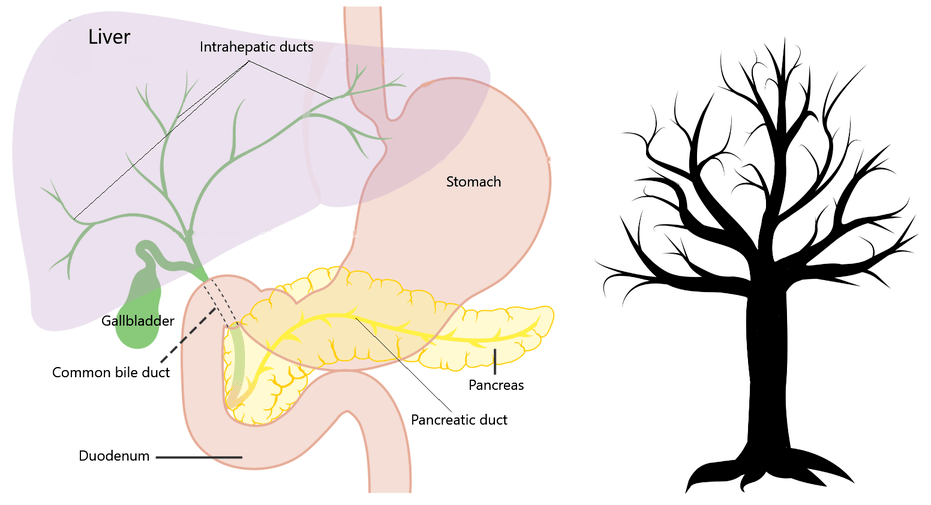
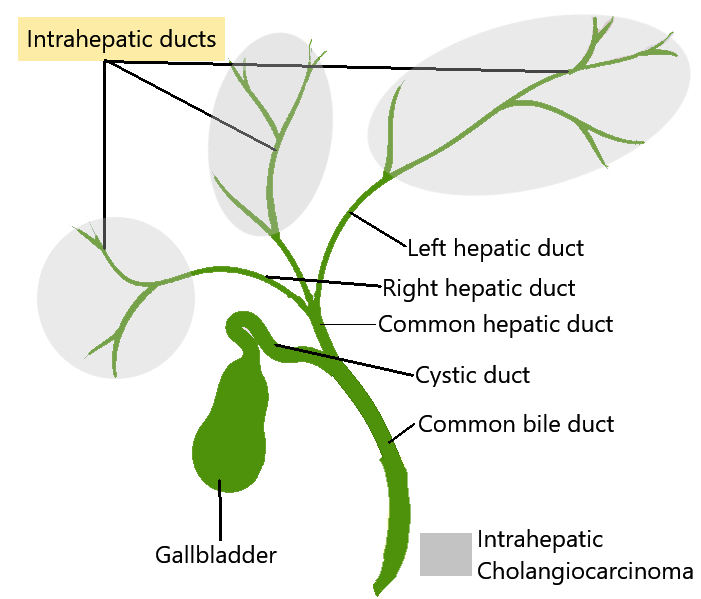
Bile is a greenish-golden yellow liquid produced by the liver for digestion of fat in the intestine. This bile is then carried from the liver to intestine by the bile duct. The bile duct is a tree-like network of tubules. It starts in the liver as smaller tubes (intrahepatic ducts) and progressively combines to form larger tubules. The branches of the right and left side of the liver coalesce to form right and left hepatic duct.
The right and left hepatic duct then join (the joint called hilum or confluence) and continues further as a single tube called common bile duct. The common bile duct goes out of the liver (extrahepatic bile duct) and joins the intestine (in the duodenum) after passing through the head of the pancreas.
Intrahepatic cholangiocarcinoma
Cholangiocarcinoma or bile duct cancer is a cancer of the bile duct. It occurs when healthy cells of the bile duct change and start growing uncontrolled. It can affect the bile duct anywhere. When it affects the bile ducts which are still in the liver (intrahepatic ducts) it is called intrahepatic cholangiocarcinoma (bile duct cancer).
The average age at which patients are diagnosed with intrahepatic cholangiocarcinoma is 70 years.
When cancer affects the joint of the left and right duct, it is called perihilar or hilar cholangiocarcinoma. While cancer affecting the part of the duct where it joins the intestine is known as distal bile duct cancer.
Risk factors or causes
A risk factor is anything that increases a person's chance of developing cancer. They do not directly cause cancer, only increases the probability of someone developing cancer.
Following factors increases the chance of someone developing the intrahepatic bile duct cancer:
- Old age
- Infection with liver flukes - Liver flukes are parasites that infect and cause liver and bile duct disease. The species causing disease in humans include Clonorchis, Opisthorchis and Fasciola.
- Primary sclerosing cholangitis (PSC) - It is an inflammatory disorder which causes scarring and blockage of bile ducts.
- Cyst of the bile duct (choledochal cyst and Caroli syndrome) - In this condition, the bile ducts gets broader and becomes like cysts.
- Cirrhosis - It is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases.
- Viral hepatitis - hepatitis B and C
- Hepatolithiasis - stones in the liver
- Nonalcoholic fatty liver disease (NAFLD) and Nonalcoholic steatohepatitis (NASH)
- Smoking and alcohol abuse
- Chemicals and toxins e.g. thorotrast, radon
Signs and symptoms of intrahepatic cholangiocarcinoma
The intrahepatic bile duct cancer grows in the liver and then spreads. The symptoms are late to occur. The disease is often detected on ultrasound of the liver done for unrelated symptoms or a routine check-up.
When they occur symptoms and signs of intrahepatic cholangiocarcinoma are:
- Pain abdomen (commonly in the right upper abdomen)
- Unexplained weight loss
- Loss of appetite
- Malaise or weakness
- Jaundice (yellowing of eyes, skin and urine)
- Itching
- Recurrent fever
- Deranged liver function test
- Fullness or lump in the right upper abdomen
Diagnosis and staging of intrahepatic cholangiocarcinoma
Intrahepatic cholangiocarcinoma has a propensity to grow insidiously. Once suspected or diagnosed with ultrasound, the following tests are done to establish the diagnosis and to stage the disease.
Blood tests: Includes routine blood tests, blood clotting parameters and liver function tests.
Tumour markers: These are substances which are elevated in the blood of patients suffering from cancers. In intrahepatic cholangiocarcinoma, CA19.9 and carcinoembryonic antigen (CEA) may be elevated.
Computed tomographic (CT) scan: This modality uses x-ray beams and computer processing to see inside. Thin cut liver protocol triple-phase CT is done to visualise cancer and the involved parts of the liver, bile ducts and adjacent vessels. It also gives information about the distant spread of the disease.
Magnetic resonance imaging: MRI uses strong magnetic fields, radio waves and computer to generate images of inside organs. This imaging modality also gives structural information about cancer, liver, bile duct and adjacent vessels.
Positron emission tomography (PET) scan: It is a functional imaging technique which is sometimes used for staging. This helps differentiate cholangiocarcinoma from tumours which have spread to the liver from other organs.
Biopsy or cytology: In this procedure, a small sample of tumour or few cells from it is obtained and examined under the microscope confirming the diagnosis. Patients may require a biopsy if the diagnosis is in doubt, or the surgery is not planned.
Upper GI endoscopy and colonoscopy: With this thin flexible tube with a camera is passed in upper and lower parts of the intestine and they are seen from inside. This is done to make sure that the tumour in the liver has not spread from any cancer in the oesophagus, stomach or colon.
Once diagnosed, the cancer is staged. Staging tells us about the current state of the tumour, its size, its location and how much it has spread to adjacent areas and to organs which are away from the site of origin. Staging helps the oncologists and surgeons formulate a treatment plan.
TNM (tumour, node and metastasis) classification developed by the American Joint Committee on Cancer (AJCC) is used for exact classification of stage and it spans from I to IV.
The extent (size) of the tumour (T): size and number of the tumour? Has cancer reached nearby structures or organs?
The spread to nearby lymph nodes (N): Has cancer spread to nearby lymph nodes? And to how many?
The spread (metastasis) to distant sites (M): Has cancer spread to distant lymph nodes or distant organs such as the peritoneum or lungs?
Broadly these tumours can be classified into
Local - the tumour is localized
Locally advanced - the tumour has spread to nearby areas
Metastatic - the tumour has spread to distant organs
Treatment of intrahepatic cholangiocarcinoma
Intrahepatic cholangiocarcinomas are best treated by surgical resection, provided the tumour is amenable to surgery. This information is available once the staging workup is completed. Unfortunately, many patients present with late-stage, unresectable disease.
Surgical management: resection
Surgical resection is the treatment of choice for intrahepatic bile duct cancer. The surgery for removal of intrahepatic cholangiocarcinoma requires removal of the bile duct and the part of the liver it is affecting. The surgical procedure to remove a part of the liver is called hepatectomy or liver resection. The joint of the left and right duct also needs excision in many cases. The bile is then made to reach intestine by joining a loop of intestine to the cut end of the bile duct of remnant liver.
Whether the tumour is amenable to surgery by partial removal of the liver depends on many factors including how much liver needs to be removed, how healthy the liver is, whether blood supply and drainage of remaining liver can be preserved and whether the amount of remaining liver is adequate (functional liver remnant – FLR).
Surgical excision is done only for those patients whose tumours have not spread to distant organs. Besides complete resection should be feasible with sufficient FLR.
Sometimes the amount of liver which needs to be removed is too big and hence the remaining liver is small and not compatible with survival. In such cases, portal vein embolization can be done a few weeks before the surgery to increase the size of the liver, which is going to remain after surgery.
If the jaundice is very high, then it needs to be brought down before the surgery by a procedure called percutaneous transhepatic biliary drainage (PTBD) or Endoscopic retrograde cholangiopancreatography (ERCP). In these procedures drainage tube is placed in the blocked bile duct, draining the bile and decreasing jaundice.
Transplant:
A liver transplant can be an option for locally advanced intrahepatic cholangiocarcinoma, which are not amenable to resection and non-metastatic.
Palliative treatment:
For tumours which are unresectable or have spread to distant organs, the palliative treatment is given. It aims at prolonging life and improving the quality of life. The option for such patients includes chemotherapy, radiotherapy and liver-directed therapy.
In chemotherapy drugs are given which kills the cancer cells temporarily. Radiotherapy is a cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumours. Liver-directed therapy can include treatment with radioembolization with yttrium-90 (Y-90), transarterial chemoembolization, and ablation, most commonly radiofrequency ablation.
Prognosis (survival rate) of intrahepatic cholangiocarcinoma
Many patients present in an advanced stage with unresectable disease. With resection, 5-year survival ranges from 10% to 49% depending on the stage and aggressiveness of the disease.
Stay Alert! Stay Healthy!
Wish you a speedy recovery!


