Ampullary Cancer
Dr. Nikhil Agrawal | Last reviewed on
The Ampulla
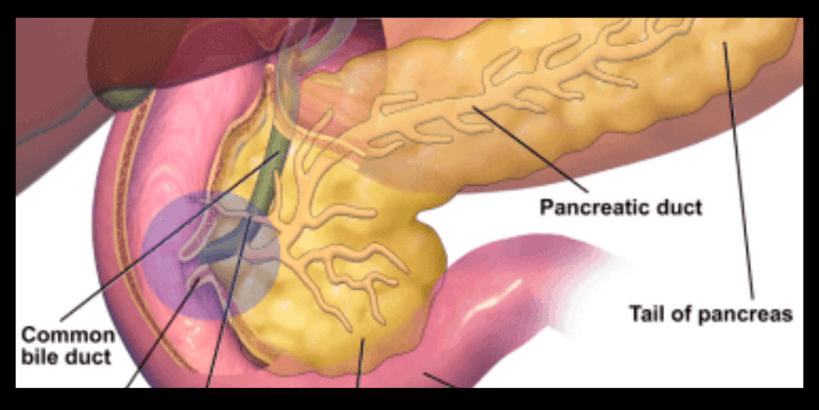
The ampulla or ampulla of Vater is a mound-like opening in the duodenum. The duodenum is a C-shaped part of the small intestine in the beginning. At the ampulla, the bile duct transporting bile from the liver and the pancreatic duct which brings pancreatic juice from the pancreas meets and then opens into the intestine.
Ampullary cancer
Ampullary cancer is a rare type of cancer. Ampullary cancer arises from the cells lining the ampulla of Vater. Most of these cancers are adenocarcinomas. Ampullary cancers present earlier and have a better prognosis than other periampullary cancers.
Periampullary cancer is a term used to refer to cancer that occurs around ampulla. This includes cancer affecting the head of the pancreas, distal bile duct (cholangiocarcinoma), duodenum, and ampulla. These cancers are grouped because they share similar clinical features and treatment options.
Risk factors for ampullary cancer
Anything that increases the risk of someone getting cancer is a risk factor. The risk factor does not directly cause the disease. Some with many risk factors will not have the disease, while some with no known risk factors will get it.
Risk factors for ampullary cancer have not been clearly defined because of the low incidence of this disease in the population. According to a case-control study, previous cholecystectomy (gallbladder removal) and use of proton pump inhibitors (medicine to suppress stomach acid) were associated with an increased risk of ampullary tumours.
Signs and symptoms of ampullary cancer
Ampullary cancers compress the bile duct, blocking the flow of bile and causing yellowing of eyes and urine called jaundice. Pale stools and itching usually accompany this. Other warning signs of ampullary cancer can be weight loss, loss of appetite and abdominal pain. Besides, ampullary cancers bleed causing black stools (melena) and anaemia.
Signs and symptoms of ampullary cancer:
- Jaundice (yellowing of skin, eyes and urine with pale stools) Itching
- Abdominal pain
- Weight loss and loss of appetite
- Recurrent vomiting
- Black stools
- Anaemia
- Fever
Diagnosis and staging of ampullary cancer
MRCP, side view endoscopy with biopsy and a CT scan or PET scan diagnose and stage ampullary cancer. Your surgeon will also do tests to quantify your jaundice and check your kidney function, haemoglobin and blood clotting parameters. A tumour marker called CA 19.9 and CEA will also be checked.
Magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP)
MRI uses strong magnetic fields, radio waves and computers to generate images of inside organs. MRCP is a type of MRI scan that is used to visualise the bile ducts and pancreatic ducts. MRCP is one of the initial investigations in patients with jaundice. This imaging modality gives a detailed view of the bile duct and pancreatic duct.
Side viewing endoscopy
It is a procedure in which a thin flexible tube is passed into your intestine through your mouth. It has a camera at the tip of the tube which is angled to the side and a view of the ampulla is taken, showing any cancerous growth.
Biopsy
If a tumour is found at the ampulla, then a small sample (biopsy) is taken and examined under a microscope confirming the diagnosis.
Endoscopic ultrasound (EUS)
It is an ultrasound of the ampullary region from the inside of your intestine. It aids diagnosis where CT/MRI do not show cancerous growth, while it is suspected.
Computed tomography (CT) scan
CT Scanner acquires images of the inside of our body with the help of X-ray beams. These images are then computer-processed, giving an accurate representation. Contrast injected into the blood enhances these images. A CT scan will show us the tumour and its extent.
Positron emission tomography (PET) scan
Cancer cells take up a larger amount of glucose. Here injected radioactive glucose (18F-fluorodeoxyglucose; FDG) binds to the tumour, and the patient is scanned. The images are computer-processed and combined with CT images, giving us a CT image with bright-coloured tumours.
Treatment of ampullary cancer
The treatment depends upon the stage of the disease and the level of jaundice. For localised disease, surgery is the best treatment. While advanced disease (unresectable and metastatic) is treated with systemic therapy (chemotherapy, targeted therapy and immunotherapy). Jaundice is treated with ERCP.
Endoscopic retrograde cholangiopancreatography (ERCP)
ERCP is a procedure to examine and access the bile duct and pancreatic duct through the ampulla. In ampullary cancer, ERCP relieves jaundice by placing a plastic or metal stent across the obstruction. Sometimes ERCP may not be possible and we may need to do a Percutaneous transhepatic biliary drainage (PTBD) to decrease the jaundice.
ERCP is done to decrease jaundice before surgery when it is high and before starting any systemic therapy.
Surgery for ampullary cancer (Whipple procedure)
Surgery is the best option and is done when the cancer is diagnosed at a stage where it can be completely removed by surgery.
The operation to remove ampullary cancer is called the Whipple operation, also known as pancreaticoduodenectomy. In this, the head of the pancreas is removed along with the duodenum, bile duct, gallbladder, part of the stomach, a small part of the small intestine and adjacent lymph nodes. To restore gastrointestinal continuity, the small intestine is then joined to the pancreas (sometimes the pancreas is joined to the stomach), the remaining bile duct and the stomach.
The 5-year survival rate of ampulla of Vater cancer after radical surgery ranges from 35.0% to 62.7%.
Treatment of locally advanced ampullary cancer
If the tumour is locally advanced, then we may give you neoadjuvant treatment (chemotherapy or chemoradiotherapy) to decrease the size of the tumour and then resect it to increase your chances of survival.
Treatment of advanced ampullary cancer
Advanced disease (unresectable and metastatic) is treated with systemic therapy (chemotherapy, targeted therapy and immunotherapy). After FNAC/biopsy and stenting (if jaundiced) chemotherapy is given. Chemotherapy uses drugs to destroy cancer cells.
If the tumour is causing blockage of the food passage, then a metal stent is placed in the food passage endoscopically. If this fails, then a bypass surgery like gastrojejunostomy will be required.
Wish you or your loved one a speedy recovery!


